Pulmonary Hypertension
WHO Classification of Pulmonary Hypertension
Group I. Pulmonary Arterial Hypertension
Idiopathic primary
Familial and related Disorders collagen vascular
disease, congenital systemic to pulmonary shunts, portal hypertension, HIV,
drugs and toxins, thyroid disorders, glycogen storage disease, Gaucher’s
disease, hereditary hemorrhagic telangiectasia, hemoglobinopa thies,
myeloproliferative disorders, splenectomy
Associated with Significant Venous or Capillary
Involvement pulmonary venoocclusive disease, pulmonary capillary
hemangiomatosis
Persistent Pulmonary Hypertension of Newborn Group II.
Pulmonary venous Hypertension left sided atrial or ventricular heart disease,
left sided valvular heart disease
Group III. Pulmonary Hypertension associated with
Hypoxemia COPD, interstitial lung disease, sleep disordered breathing, alveolar
hypoventilation disorders, chronic exposure to high altitude, developmental
abnormalities
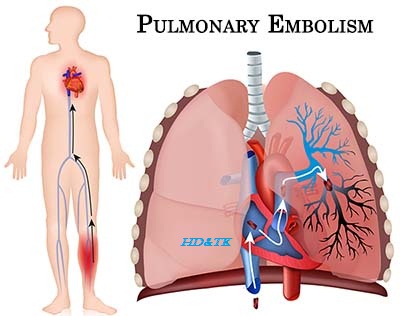
Group IV. Pulmonary Hypertension due to chronic
Thrombotic Diseases or Both thromboembolic obstruction of proximal pulmonary
arteries, thromboembolic obstruction of distal pulmonary arteries, pulmonary
embolism (tumor, parasites, foreign material)
Group V. Mi8scellaneous sarcoidosis, pulmonary
Langerhans cell histiocytosis, lymphangiomatosis, compression of pulmonary
vessels (adenopathy, tumor, fibrosing mediastinitis)
Pathophysiology
Definition of
Pulmonary Hypertension mean pulmonary arterial pressure (PAP) >25 mmHg at
rest or mean PAP >30 mmHg with exercise measured with right heart
catheterization
Clinical
Features
History unexplained dyspnea on exertion, cough,
chest pain, hemoptysis, dizziness, syncope, hoarseness, past medical history
(cardiac and respiratory diseases, thromboembolic diseases, HIV, cirrhosis,
autoimmune and rheumatologic dis orders), medications (amphetamine, diet pill
such as dexfenfluramine)
Physical vitals (tachypnea, tachycardia, atrial
fibrillation, hypoxemia), peripheral cyanosis, small pulse volume, elevated JVP
(prominent a wave or absent if atrial fibrillation, large v wave), right ventri
cular heave, palpable P2, narrowly split or paradoxi cally split S2, right
sided S4, tricuspid regurgitation
murmur, Graham Steell murmur (high pitched,
decrescendo diastolic rumble over LUSB), crackles, congestive liver, ascites,
ankle edema
Investigations
Basic
Labs CBCD, electrolytes, urea, Cr, AST, ALT, ALP,
bilirubin, INR, albumin, ANA, RF, anti CCP, anti SCL 70, anticentromere
antibody, ESR, HIV serology, TSH
Imaging CXR, CT chest, V/Q scan or CT chest PE
protocol, echocardiogram
ECG
Overnight Polysomnography if suspect OSA
ABG
PFT
Special
Right Heart Catherization
Management
Symptoms of Control O2, calcium channel blockers if
positive vasoreactivity test (high doses), vasodilators (prostacyclin,
sildenafil, bosentan, NO), anticoagulation
Treatment Treatments include
conventional medical therapies and oral, Depending on the severity of PH, heart
or lung transplant may also be an option
Atrial Septostomy
Lung Transplant
Specific
Entities
Eisenmenger Syndrome left to right shunt
leading to pulmonary hypertension and eventually right to left shunt
Thyrotoxic Associated Pulmonary
Hypertension pulmonary artery hypertension and isolated right sided heart
failure are associated with hyperthyroidism. Restoration to a euthyroid state
may reverse pulmonary hypertension



Comments
Post a Comment