Pleural Effusion
Pleural
effusion, sometimes referred to as “water on the lungs,” is the
build-up of excess fluid between the
layers of the pleura outside the lungs. The pleura are thin
membranes that line the lungs and the inside of the chest cavity and act to
lubricate and facilitate breathing.
Differential
Diagnosis
Exudative malignancy,
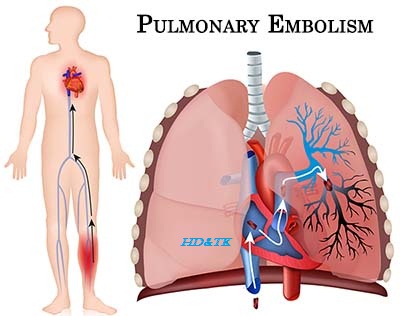
infections, connective tissue disease, pulmonary embolism, hemothorax,
pancreatitis, chylothorax
Trabsydatuve HF,
hypoalbuminemia (GI losing enteropathy, cirrhosis, nephrotic syndrome, malnutrition),
SVC obstruction, hepatohydrothorax, urinothorax, atelectasis, trapped lung,
peritoneal dialysis, hypothyroidism, pulmonary embolism Note: pulmonary
embolism, malignancy, and sar coidosis can present as either exudative or
transudative effusions. HF following diuresis may become ‘‘pseudo exudative’’
(check albumin gradient)
Clinical
Features
History dyspnea, cough,
hemoptysis, chest pain, weight loss, fever, trauma, occupational exposures,
past medical history (pneumonia, liver disease, kidney disease, thyroid
disease, cancer, HF, thromboembolic disease, connective tissue disease,
smoking), medications
Physical vitals, cyanosis,
clubbing, tracheal deviation away from side of effusion (if no collapse or
trapped lung), peripheral lymphadenopathy, Horner’s syndrome, respiratory
examination (decreased breath sounds and tactile fremitus, stony dullness to
percussion), cardiac examination, leg swelling (HF or DVT)
Rational Clinical Examination Series Does the patient have Pleural
Effusion?
Auscultatory Percussion auscultate with the
diaphragm of the stethoscope over the posterior chest wall while gently tapping
over the manubrium with the distal phalanx of one finger. Diminished resonance
suggests effusion
Sens
|
Spc
|
LR+
|
LR
|
|
Physical
|
||||
Asymmetric chest expansion
|
74%
|
91%
|
8.1
|
0.29
|
Auscultatory percussion
|
77%
|
92%
|
7.7
|
0.27
|
Crackles
|
56%
|
62%
|
1.5
|
0.71
|
Diminished breath sounds
|
42 88%
|
83 90%
|
4.3 5.2
|
0.15 0.64
|
Dullness to conventional percussion
|
73%
|
91%
|
8.7
|
0.31
|
Pleural friction rub
|
5.30%
|
99%
|
3.9
|
0.96
|
Reduced tactile fremitus
|
82%
|
86%
|
5.7
|
0.21
|
Reduced vocal resonance
|
76%
|
88%
|
6.5
|
0.27
|
APPROACH ‘‘dullness to percussion and
tactile fremitus are the most useful findings for pleural effusion. Dull
chest percussion makes the probability of a pleural effusion much more likely
but still requires a CXR to confirm the diagnosis. When the pretest
probability of pleural effusion is low, the absence of reduced tactile
fremitus makes pleural effusion less likely so that a CXR might not be
necessary depending on the overall clinical situation’
|
||||
Investigations
Basic
Labs CBCD, electrolytes, urea, Cr, LDH,
total protein, AST, ALT, ALP, bilirubin, INR, PTT, albumin
Imaging CXR (PA, lateral, decubitus), CT
chest
Thoracentesis send pleural fluid for
cell count and differential, Gram stain, C&S, AFB and fungal cultures, LDH,
total protein, pH, and cytology. Under special circumstances, also consider amylase,
glucose, cholesterol, adenosine deaminase (for TB), albumin
Special
Biopsy closed pleural biopsy, medical
thoracoscopy, bronchoscopy, surgical biopsy (video assisted thoracic surgery)
Diagnostic
Issues
Overall Approach
generally, if the effusion is >1/4 of hemithorax, enough fluid is present
for diagnostic thoracentesis; obtain decubitus film to assess for loculation.
In the absence of loculation, and with >10 mm [0.4 in.] layering of fluid on
decubitus film, bedside thoracentesis can be attempted; otherwise, request U/S
guided thora centesis. If only a small amount of fluid is present (<10 mm [><0.4 in.]) and/or HF suspected, start with diuresis for 2 to 3 days. If no improvement, perform thoracentesis to distinguish between transudative and exudative causes ><10
mm <0.4 in.]) and/or HF suspected,
start with diuresis for 2 3 days. If no improvement, perform thoracentesis to
distinguish between transudative and exudative causes
Light's Criteria for Exudative Effusion
Any one of the following criteria would
suggest exudative effusion: fluid/serum total protein ratio >0.5,
fluid/serum LDH ratio >0.6, fluid LDH >2/3 upper limit of normal serum
level
Pleural
Fluid Analysis
Pleural Fluid Analysis Fluid Acidosis (pH
<7.2) complicated parapneumonic, TB, paragonimiasis, malignancy, rheumatoid
arthritis, SLE, hemothorax, esophageal rupture Fluid Glucose (<3.3 mmol/L [< 60 mg/dL]) para pneumonic, TB,
paragonimiasis, malignancy, rheu matoid arthritis, Churg Strauss, hemothorax
Fluid Eosinophilia (>10%)
paragonimiasis, malignancy, Churg Strauss, asbestos, drug reac tion, pulmonary
embolism, hemothorax, pneumothorax, idiopathic (20%)
Cytology
for Malignancy
the yield for diagnosis with single attempt is 60%, two attempts is 85%, three
attempts is 90 95%; obtain as much fluid as possible to increase diagnostic
yield
Fluid for AFB obtain as much fluid as
possible and ask laboratory to centrifuge collection and to culture sediment to
increase diagnostic yield
Management
Symptoms Control O2, diuresis
(furosemide), drainage (thoracentesis, pigtail catheter, PleurX catheter, chest
tube), pleurodesis (talc slurry or poudrage), surgery (talc slurry,
pleuroperitoneal shunt, pleural abrasion, pleurectomy)
Treatment
Diuretics and
other heart failure medications are used to treat pleural effusion caused by
congestive heart failure or other medical causes. A malignant effusion may
also require treatment with chemotherapy, radiation therapy or a medication
infusion within the chest.
Specific
Entities
Parapneumonic Effusion
Uncomplicated exudative effusion that
resolves with resolution of pneumonia. Generally disappears with antibiotics
alone
Complicated persistent bacterial
invasion and fluid collection. Characterized by pleural fluid acidosis but
sterile fluid. Pleural loculation may occur as fibrin gets deposited from
inflammation.
Empyema presence of bacteria in Gram
stain or pus in drainage (culture not necessary). pH often < 7.2. For
unloculated fluid, chest tube/small bore catheter drainage usually adequate.
For loculated effusions, thrombolytics such as streptokinase or TPA could be
considered. Thoracoscopy represents an alternative to fibrinolytics. Open
decortication is the last resort
Traped Lung stable chronic effusion,
especially with history of pneumonia, pneumothorax, thoracic surgery or
hemothorax. Diagnosis is established by measuring negative change in
intrapleural pressure during thoracentesis. Treat by lung re expansion,
sometimes requiring thoracotomy with decortications
Hepatohydrothorax suspect if
cirrhosis and portal hypertension, even in the absence of ascites. Pleural
effusion results from passage of peritoneal fluid into pleura because of
negative intrathoracic pressures and diaphragmatic defects. Do not insert chest
tube. Treat with diuresis, salt restriction, and consider liver
transplantation/TIPS procedure.



I love the focus on comprehensive care, including therapy and medication management. This truly addresses the whole person.
ReplyDeleteBrainpower Wellness Institute
The team at Renewed Mental Health Group appears to be incredibly knowledgeable and caring. It’s evident that they prioritize the well-being of their clients.
ReplyDeleteRenewed Mental Health Group