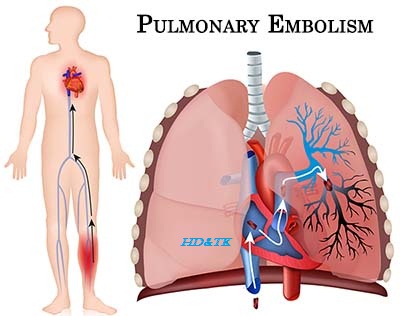
Pulmonary Embolism
Pulmonary embolism is the sudden
blockage of a major blood vessel (artery) in the lung, usually by a
blood clot. In most cases, the clots are small and are not deadly, but they can
damage the lung. But if the clot
is large and stops blood flow to the lung, it can be deadly.
Differential
diagnosis of acute Dyspnea
Respiratory
Airway
COPD exacerbation, asthma exacerbation, acute bronchitis, infectious
exacerbation of bronchiectasis, foreign body obstruction
Parenchyma pneumonia, cryptogenic organizing pneumonia, ARDS, acute exacerbation of
interstitial lung disease
Vascular
pulmonary embolism, pulmonary hypertension
Pleural
pneumothorax, pleural effusion
Cardiac
Myocardial
HF exacerbation, myocardial infarction
Valvular
aortic stenosis, acute aortic regurgitation, endocarditis
Pericardial
pericardial effusion, Tamponade
Systemic
sepsis, metabolic acidosis, anemia
Others
neuromuscular, psychogenic, anxiety
Pathophysiology
Virchow’s
Triad risk factors for venous thrombo embolism
Injury
fracture of pelvis, femur, or tibia
Hypercoaguability
obesity, pregnancy, estrogen, smoking, cancer (high suspicion of occult malignancy
in patients who develop pulmonary embolism while on anticoagulation),
autoimmune dis orders (anticardiolipin antibody syndrome, lupus anticoagulant,
IBD), genetics (history of DVT/PE, factor V Leiden, antithrombin III
deficiency, protein C/S deficiency, prothrombin G20210A mutation, hyperhomocysteinemia)
Stasis surgery requiring >30 min of anesthesia, prolonged immobilization, CVA, HF
Clinical
Features
History
dyspnea (sudden onset), pleuritic chest pain, cough, hemoptysis, pre/syncope,
unilateral leg swelling/ pain, past medical history (previous DVT/PE, active
cancer, immobilization or surgery in last 4 weeks, miscarriages), medications
(birth control pill, anticoagulation)
Physical
vitals (tachycardia, tachypnea, hypotension, fever, hypoxemia), respiratory
examination (pulmonary hypertension if chronic PE), cardiac examination (right
heart strain), leg swelling
Investigations
Basic
Labs
CBCD, electrolytes, urea, Cr, PTT, INR, troponin/CK 3, D dimer (if low
probability for PE or outpatient), βhCG in women of reproductive age
Imaging CXR, duplex U/S of legs, V/Q scan, CT chest (PE protocol)
ECG
may see normal sinus rhythm (most common), sinus tachycardia (most common
abnormality), atrial fibrillation, right ventricular strain (T wave inversion
in anterior precordial leads), non specific ST T wave changes, right axis deviation,
right bundle branch block and/or S1Q3T3 (tall S wave in lead I, Q wave and
inverted T wave in lead III)
ABG
if respiratory distress
Special
Echocardiogram
to check for right heart strain (dilated RV and elevated RVSP). Particularly
important if hemodynamic changes
Pulmonary
Angiogram gold standard
Thrombophilia
Workup factor V Leiden, pro thrombin G20210A, anticardiolipin antibody, lupus
anticoagulant, protein C, protein S, antithrombin III, fibrinogen; consider
homocysteine level and workup for paroxysmal nocturnal hemoglobinuria and
antiphospholipid syndrome in cases of combined arterial venous thrombosis.
Diagnostic
Issues
CXR
Findings in Pulmonary Embolism normal, atelectasis, unilateral small pleural
effusion, enlarged central pulmonary artery, elevated hemidiaphragm,
Westermark’s sign (abrupt truncation of pulmonary vessel), Hampton’s hump
(wedge infarct)
D
DIMER (sens 85 96%, spc 45 68%, LR+ 1.7 2.7, LR 0.09 0.22) can rule out PE if
low clinical suspicion
V/Q
Scan (sens high, spc high) useful but result often not definitive (intermediate
probability) because of other intraparenchymal abnormalities
CT
PE PROTOCOL (sens 57 100%, spc 78 100%) can be very helpful as it provides clues
to other potential diagnoses/pathologies as well. Not good for subseg mental
pulmonary emboli
Leg
Vein Doppler (sens 50%, spc moderate) serial dopplers may be used for diagnosis
of DVT if CT or V/Q scan failed to demonstrate PE but clinical suspicion still
high
Well’s
Criteria for Pulmonary Embolism Scoring signs/symptoms of DVT (+3), alternative
diagnosis less likely (+3), HR >100 (+1.5), immobilization or surgery in
last 4 weeks (+1.5), previous DVT/PE (+1.5), hemoptysis (+1), active cancer
(+1)
Low
Suspicious (sum 0 1, <10% chance) D dimer ͢if positive, CT or V/Q scan Intermediate SUSPICION (sum 2 6, 30% chance)
D dimer ͢ CT or V/Q scan ͢ if negative but suspicious, leg doppler ͢ if negative but still sus picious, pulmonary angiogram
High
Suspicious (sum >6, >70% chance) CT or V/Q scan ͢ if negative but suspicious, leg Doppler ͢ if negative but still suspicious, pulmonary
angiogram
Management
Acute
ABC, O2 to keep sat >94%, IV, consider thrombolysis (must be done in ICU)
for massive PE (hemodynamic instability, right ventricular strain)
Anticoagulation
if moderate to high risk of developing PE, consider initiating anticoagulation
while waiting for investigations. Heparin (unfractionated heparin 5000 U IV
bolus, then 1000 U/h and adjust to 1.5 2.5 normal PTT), LMWH (enoxaparin 1
mg/kg SC BID or 1.5 mg/kg SC daily), or fondaparinux 5 mg SC daily (<50 kg), 7.5 mg SC daily (50 100 kg), or 10 mg SC daily (>100
kg). Start warfarin 5 mg PO daily within 72 h and continue
heparin/LMWH/fondaparinux until INR is between 2 and 3; ensure overlap of
heparin and coumadin with therapeutic INR for at least 48 h
Thrombolytics
controversial as increased risk of intracranial bleed and multiple
contraindications (see below). Consider only if hemodynamically unstable or
life threatening pulmonary embolism. TPA 100 mg IV over 2 h, or streptokinase
250,000 IU over 30 min, the 100,000 IU/h over 12 24 h or 1.5 million IU over 2
h. Unfractionated heparin may be used concurrently
Surgical
embolectomy. Consider if thrombolysis failed or contraindicated or if hemodynamically
unstable
IVC
Filter if anticoagulation contraindicated
Treatment Issues
Contraindications
to Thrombolytic Therapy Absolute Contraindications history of hemorrhagicstroke
or stroke of unknown origin, ischemic stroke in previous 3 months, brain
tumors, major trauma in previous 2 months, intra cranial surgery or head injury
within 3 weeks
Relative
Contraindications TIA within 6 months, oral anticoagulation, pregnancy or
within 1 week postpartum, non compressible puncture sites, traumatic CPR,
uncontrolled hypertension (SBP >185 mmHg, DBP > 110 mmHg), advanced liver disease,
infective endocarditis, active peptic ulcer, thrombocytopenia
Anticoagulation
Duration
First
Pulmonary Embolism with reversible or Time-limited Risk Factor anticoagulation
for at least 3 months
Unprovoked
PE at least 3 months of treatment. If no obvious risk factors for bleeding,
consider indefinite anticoagulation
PE
and malignancy treatment with SC LMWH better than oral warfarin. Treatment
should be continued until eradication of cancer as long as there are no
significant contraindications to anticoagulation
PE
and Pregnancy SC LMWH is preferred for outpatient treatment. Total duration of
therapy should be 6 months unless patient has risk factors for hypercoagulable
state
Specific Entities
Fat
Embolism
Pathophysiology
embolism of fat globules to lungs, brain, and other organs metabolized to
fatty acids leading to inflammatory response. Commonly caused by closed
fractures of long bones, but may also occur with pelvic fractures, orthopedic
procedures, bone marrow harvest, bone tumor lysis, osteomyelitis, liposuction,
fatty liver, pancreatitis, and sickle cell disease
Clinical
Features triad of dyspnea, neurological abnormalities (confusion), and
petechial rash (head and neck, chest, axilla). May also have fever,
thrombocytopenia, and DIC
Diagnosis
clinical diagnosis (rash is pathognomonic). Investigations may include CXR, V/Q
scan, CT chest, and MRI head
Treatments
supportive care as most patients will fully recover. Mortality is 10%. Primary
prophylaxis includes early mobilization and maybe steroids



Comments
Post a Comment