Cardiac Diseases and Treatment
Aortic Dissection
Differential Diagnosis
Cardiac
Myocardial infarction, angina
Valvular aortic stenosis, aortic
regurgitation
Pericardial Pericarditis
Vascular aortic dissection
Respiratory
Parenchymal pneumonia, cancer
Pleural pneumothorax, pneumomediasti
num, pleural effusion, pleuritis
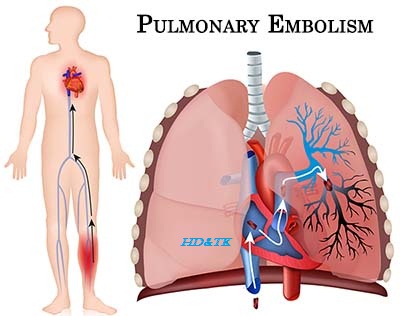
Vascular pulmonary embolism, pulmonary
hypertension
GI esophagitis, esophageal cancer, GERD,
peptic ulcer disease, Boerhaave’s, cholecystitis, pancreatitis OTHERS
musculoskeletal, shingles, anxiety
Pathophysiology
Aanatomy layers of aorta include intima,
media, and adventitia. Majority of tears found in ascending aorta right lateral
wall where the greatest shear force upon the artery wall is produced.
Aortic Tear and Extension aortic tear
may produce a tearing, ripping sudden chest pain radiating to the back. Aortic
regurgitation can produce diastolic murmur. Pericardial tamponade may occur,
leading to hypotension or syncope. Initial aortic tear and subsequent extension
of a false lumen along the aorta may also occlude blood flow into any of the
following vascular structures:
Coronary acute myocardial infarction
(usually RCA)
Brachiocephalic, Left Subclavian, Distal
Aorta, absent or asymmetric peripheral pulse, limb ischemia RENAL anuria, renal
failure.
Carotid syncope/hemiplegia/death
Anterior Spinal paraplegia/quadriplegia,
anterior cord syndrome
Classification Systems
Stanford A ¼ any ascending aorta
involvement, B ¼ all others
Debakey I ¼ ascending and at least
aortic arch, II ¼ ascending only, III ¼ originates in descending and extends
proximally or distally
Risk Factors
Common hypertension, age, male
Vascular Takayasu arteritis, giant cell
arteritis, rheumatoid arthritis, syphilitic aortitis
Collagen Disorders Marfan syndrome,
Ehlers Danlos syndrome, cystic medial necrosis
Valvular bicuspid aortic valve, aortic
coarctation, Turner syndrome, aortic valve replacement
Other cocaine, trauma
Clinical
Features
Rational Clinical Examination series
Does this patient have an acute thoracic Aortic Dissection?
LR+
|
LR
|
|
History
|
||
Hypertension
|
1.6
|
0.5
|
Sudden chest pain
|
1.6
|
0.3
|
Tearing or ripping pain
|
1.2 10.8
|
0.4 0.99
|
Physical
|
||
Pulse deficit
|
5.7
|
0.7
|
Focal neurological deficit
|
6.6 33
|
0.71 0.87
|
Diastolic murmur
|
1.4
|
0.9
|
CXR/ECG
|
||
Enlarged aorta or wide mediastinum
|
2.0
|
0.3
|
LVH on ECG
|
0.2 3.2
|
0.84 1.2
|
Approach ‘‘presence of tearing,
ripping, or migrating pain may suggest dissection. Pulse deficit or focal
neurological deficits greatly increase likelihood of dissection. Absence of
pain of sudden onset decreases likelihood of dissection. Normal aorta and
mediastinum on CXR help to exclude diagnosis’’
|
||
Investigations
Basic
ASIC LABS CBCD, electrolytes,
urea, Cr, troponin/CK 3, glucose, AST, ALT, ALP, bilirubin, albumin, lipase, INR/PTT
Radiography CXR, echocardiogram (TEE), CT chest or MRI chest
ECG
Special
Aortography
Diagnostic and Prognostic Issues
CXR Findings wide mediastinum (>6 cm
[2.4 in.]), indistinct aortic knuckle, pleural cap, difference in diameter
between ascending and descending aorta, blurring of aortic margin secondary to
local extravasation of blood, pleural effusion or massive hemothorax, displaced
calcification (separation of the intimal aortic calcification from the edge of
the aortic shadow >1 cm [0.4. in.])
Prognosis
TYPE A with surgery, 1 month survival 75
80%, 10 year survival 55%
TYPE B with aggressive hypertensive
treatment, 1 month survival >90%, 10 year survival 56%
Management
ABC O2 to keep sat >95%, IV,
antihypertensive (keep HR <120 mmHg. Labetalol 2 mg/ min IV loading drip,
then 2 8 mg/min (target heart rate 55 60) or 20 80 mg IV q10min, maximum 300
mg, then 200 400 mg PO BID. If SBP still >100 mmHg, sodium nitroprusside
0.25 0.5 mg/kg/ min IV initially, then 0.25 10 mg/kg/min)
Treatment
Type A (emergent surgical repair,
endovascular stenting, long term blood pressure control).
Type B (medical blood pressure control).
Monitor over time with serial CT/MR chest.




Comments
Post a Comment