Heart Failure
Differential
Diagnosis of HF Exacerbation/ Dyspnea
Cardiac
Myocardial HF exacerbation, myocardial
infarction
Valvur aortic stenosis, acute aortic
regurgitation, mitral regurgitation/stenosis, endocarditis
Pericardial Tamponade
Dysrhythmia
Respiratory
Airway COPD exacerbation, asthma
exacerbation, acute bronchitis, bronchiectasis, foreign body obstruction
Parenchyma pneumonia, cryptogenic
organizing pneumonia, ARDS, interstitial lung disease exacerbation
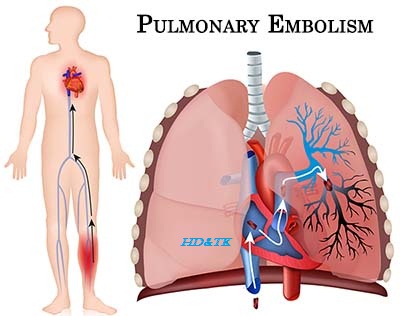
Vascular pulmonary embolism, pulmonary
hypertension
Pleural pneumothorax, pleural effusion
Systemic sepsis, ARDS, metabolic
acidosis, anemia, neuromuscular, psychogenic, anxiety.
Pathophysiology
Anatomic/Physiologic
Classification of Cardiomyopathy
Dilated (dilatation and impaired
contraction of one or both ventricles) idiopathic, ischemic, valvular, viral,
genetic, late manifestation of hypertrophic heart disease, tachycardia induced,
alcohol induced, peripartum.
Hhypertrophic (disorder with
disproportionate hypertrophy of the left ventricle and occasionally right
ventricle) idiopathic (autosomal dominant inheritance with incomplete
penetrance), storage disease (Fabry’s disease, Pompe disease, Hurler’s
syndrome, Noonan’s syndrome), athlete’s heart, obesity, amyloid.
Restrictive (non dilated ventricles with
impaired ventricular filling) idiopathic familial, infiltrative (amyloidosis,
hemochromatosis, sarcoidosis), drugs, radiation, endomyocardial fibrosis.
Arrhythomogenic Right Ventricular
(replacement of right ventricular free wall with fatty tissue) arrhythmogenic
RV dysplasia.
Unclassifiable endocardial
fibroelastosis, left ventricular non compaction
Etiologic
Classification of Cardiomyopathy
Ischemic Cardiomyopathy (mostly dilated)
varying degrees of persistent ischemia, infarction, and left ventricular
remodeling.
Valvular Cariomyopathy (mostly dilated)
abnormal loading conditions and secondary left ventricular remodeling and
dysfunction.
Hypertensive Cardiomyopathy (dilated,
restrictive) left ventricular hypertrophy and dysfunction.
Diabetic Cardiomyopathy (dilated) left
ventricular dysfunction in the absence of atherosclerosis or hypertension.
Inflammatory Cardiomyoathy (mostly
dilated) infectious (diphtheria, rheumatic fever, scarlet fever, typhoid fever,
meningococcal, TB, Lyme disease, Leptospirosis, RMSF, poliomyelitis, influenza,
mumps, rubella, rubeola, variola, varicella, EBV, Coxsackie virus, echovirus,
CMV, hepatitis, rabies, mycoplasma, psittacosis, arboviruses, histoplasmosis,
cryptococcosis, Chagas disease), autoimmune, idiopathic myocardial inflammatory
diseases.
Metabolic Cardiomyopathy (dilated,
restrictive, and/or hypertrophic) endocrine (thyrotoxicosis, hypothyroidism,
acromegaly, pheochromocytoma), storage diseases (glycogen storage disease,
Fabry’s disease, Gaucher’s disease, Niemann Pick disease), nutritional
deficiencies (Beriberi, Kwashiorkor, pellagra), deposition (amyloidosis,
hemochromatosis, sarcoidosis).
Muscular Dystrophies (mostly dilated)
Duchenne, Becker’s, myotonic dystrophy.
Neuromuscular Friedreich’s ataxia (hyper
trophic), Noonan’s syndrome, lentiginosis.
General Systemic Disease (mostly
dilated) connective tissue diseases (rheumatoid heart disease, ankylosing
spondylitis, SLE, scleroderma, der matomyositis), granulomatous (sarcoidosis,
Wegener’s granulomatosis, granulomatous myocarditis), other inflammatory (giant
cell myocarditis, hypersensitivity myocarditis), neoplasm (pri mary, secondary,
restrictive pattern).
Sensitivity and Toxic Reactions (mostly
dilated) alcohol, amphetamine, arsenic, catecholamines, cocaine,
anthracyclines, zidovudine, radiation (restrictive as well).
Functional
Classification of Heart Failure
Systolic Dysfunction (lower LVEF <
45%) S3 (dilated ventricle with volume overload). Mechanisms include decreased
contractility and increased afterload. Causes include MI, cardiomyopathy
(dilated, infiltrative), valvular (aortic regurgitation, mitral regurgitation,
burn out aor tic stenosis), burn out hypertension and Myocarditis.
Diastolic Dysfunction (normal LVEF) S4
(stiff ventricle), LVH, lower ventricular relaxation, normal LVEF, raised
chamber pressures. Mechanisms include decreased active relaxation and passive
relaxation (stiff ventricle). Causes include ischemia, hypertension, valvular
(aortic stenosis), cardio myopathy (restrictive, hypertrophic), and pericardial
disease.
Mixed Dysfunction in many cases,
diastolic dys function is present with systolic heart failure.
Precipitants
of the HF *Heart Failure*
Forget to take medications (non
adherence).
Arrhythmia, anemia.
Infection, ischemia, infarction.
Lifestyle change.
Upregulators (thyroid, pregnancy).
Rheumatic heart disease, acute valvular
disease.
Embolism.
Clinical Features
Distinguishing
Features Between COPD and HF
|
||
COPD
|
Heart Failure
|
|
History
|
Previous COPD Medications
|
Previous HF Medications
|
Inspect
|
Nicotine stain, barrel chest Laryngeal
height <4cm
|
|
Cardiac exam
|
Subxyphoid cardiac pulse
|
Elevated JVP, S3, S4
|
Resp. exam
|
Hyperresonance
Prolonged expiratory time
|
|
Investigations
|
CXR shows hypeinflation
ABG shows hypercapnia and hypoxemia
|
CXR shows redistribution and
cardiomegaly
ABG shows hypoxemia
Elevated BNP
|
Left Heart Failure left sided S3, rales,
wheezes, tachypnea. Causes include previous MI, aortic stenosis, and left sided
endocarditis.
Right Heart Failure right sided S3,
raised JVP, ascites, hepatomegaly, peripheral edema. Causes include left heart
failure, pulmonary hypertension, right ventricular MI, mitral stenosis, and
right sided endocarditis.
Grading of Pitting Edema 0= no edema, 1=
trace edema, 2= moderate edema disappears in 10 15 s, 3= stretched skin, deep
edema disappears in 1 2 min, 4= stretched skin, fluid leaking, very deep edema
present after 5 min
Rational
clinical examination series: Does this dyspneic patient in emergency
department have congestive heart hear failure??
|
||||
Sensation
|
Spc
|
LR+
|
LR
|
|
History
|
||||
Initial clinical judgment
|
61%
|
80%
|
4.4
|
0.45
|
Hx heart failure
|
60%
|
90%
|
5.8
|
0.45
|
Myocardial infarction disease
|
40%
|
87%
|
3.1
|
0.69
|
Coronary artery
|
52%
|
70%
|
1.8
|
0.68
|
Dyslipidemia
|
23%
|
87%
|
1.7
|
0.89
|
Diabetes
|
28%
|
83%
|
1.7
|
086
|
Hypertension
|
60%
|
56%
|
1.4
|
0.71
|
Smoker
|
62%
|
27%
|
0.84
|
1.4
|
COPD
|
34%
|
57%
|
0.81
|
1.1
|
PND
|
41%
|
83%
|
2.6
|
0.70
|
Orthopnea
|
50%
|
77%
|
2.2
|
0.65
|
Edema
|
51%
|
76%
|
2.1
|
0.64
|
Dyspnea on exertion
|
84%
|
34%
|
1.3
|
0.48
|
Fatigue and weight gain
|
31%
|
70%
|
1.0
|
0.99
|
Cough
|
36%
|
61%
|
0.93
|
1.0
|
Physical
|
||||
S3
|
13%
|
99%
|
11
|
0.88
|
AJR
|
24%
|
96%
|
6.4
|
0.79
|
JVD
|
39%
|
92%
|
5.1
|
0.66
|
Rales
|
60%
|
78%
|
2.8
|
0.51
|
Any murmur
|
27%
|
90%
|
2.6
|
0.81
|
Lower extremity edema
|
50%
|
78%
|
2.3
|
0.64
|
Valsalva maneuver
|
73%
|
65%
|
2.1
|
0.41
|
SBP < 100 mmHg
|
6%
|
97%
|
2.0
|
0.97
|
S4
|
5%
|
97%
|
1.6
|
0.98
|
SBP > 150 mmHg
|
28%
|
73%
|
1.0
|
0.99
|
Wheezing
|
22%
|
58%
|
0.52
|
1.3
|
Ascites
|
1%
|
97%
|
0.33
|
1.0
|
CXR
|
||||
Pulmonary venous
Congestion
|
54%
|
96%
|
12
|
0.48
|
Interstitial edema
|
34%
|
97%
|
12
|
0.68
|
Alveolar edema
|
6%
|
99%
|
6.0
|
0.95
|
Cardiomegaly
|
74%
|
78%
|
3.3
|
0.33
|
Pleural effusions
|
26%
|
92%
|
3.2
|
0.81
|
Any edema
|
70%
|
77%
|
3.1
|
0.38
|
Pneumonia
|
4%
|
92%
|
0.50
|
1.0
|
Hyperinflation
|
3%
|
92%
|
0.38
|
1.1
|
ECG
|
||||
Atrial fibrillation
|
26%
|
93%
|
3.8
|
0.79
|
New T wave changes
|
24%
|
92%
|
3.0
|
0.83
|
Any abnormal finding
|
50%
|
78%
|
2.2
|
0.64
|
ST elevation
|
5%
|
97%
|
1.8
|
0.98
|
ST depression
|
11%
|
94%
|
1.7
|
0.95
|
BNP
|
||||
BNP > 100 pg/mL
|
4.1
|
0.09
|
||
For patients with an estimated GFR of 15 60 mL/min/1.73 m2 , a
threshold of 201 pg/mL can be used
|
||||
Approach ‘‘the features evaluated in more than
one study with the highest LRs (>3.5) for diagnosing heart failure were
the following: the overall clinical judgment, history of heart failure, S3,
jugular venous distension, pulmonary venous congestion or interstitial edema
on CXR, and atrial fibrillation on ECG. The features evaluated in more than
one study with the lowest LRs (<0.60) for diagnosing of heart failure were the following: the overall clinical judgment, no prior history of heart failure, no dyspnea on exertion, the absence of rales, and the absence of radiographic pulmonary venous congestion, or cardiomegaly. The single finding that decreased the likelihood of heart failure the most was a BNP ><100 pg/mL. While the findings of this study are useful when assessing dyspneic patients suspected of having heart failure, no individual feature is sufficiently powerful in isolation to rule heart failure in or out. Therefore, an overall clinical impression based on all available information is best. If the appropriate constellation of findings with high LRs for heart failure are present, that may be sufficient to warrant empirical treatment without further urgent investigations’’><0.60)
for diagnosing of heart failure were the following: the overall clinical
judgment, no prior history of heart failure, no dyspnea on exertion, the
absence of rales, and the absence of radiographic pulmonary venous
congestion, or cardiomegaly. The single finding that decreased the likelihood
of heart failure the most was a BNP < 100 pg/ml. While the findings of
this study are useful when assessing dyspneic patients suspected of having
heart failure, no individual feature is sufficiently powerful in isolation to
rule heart failure in or out. Therefore, an overall clinical impression based
on all available information is best. If the appropriate constellation of
findings with high LRs for heart failure are present, that may be sufficient
to warrant empirical treatment without further urgent investigations’’
|
||||
Rational clinical
examination series Does this patient have abnormal central venous pressure?
JVP vs. Carotid JVP has biphasic
waveforms, is non palpable, is occludable, decreases with inspiration,
changes with position, and increases with abdominojugular reflux (AJR). To
perform the AJR, the blood pressure cuff is pumped 6 x and then pressed
against the abdomen at 20 35 mmHg for 15 30 s. Normal = no change in JVP, or
transient increase of >4cm 4 cm that returns to baseline before 10 s, or
sustained increase <3 cm throughout. Positive AJR occurs when abdominal
compression causes a sustained increase in JVP >4cm (sens 24%, spc 96%,
LR+ 6.4)
Approach ‘‘once the JVP is identified, measure
the
vertical height. A distance >4 cm above
the sternal angle is considered abnormal (i.e. CVP >9cmH2O). An
assessment of low JVP has an LR+ for low CVP of 3.4, while an assessment of
high JVP has an LR+ for high CVP of 4.1’’
|
||||
Rational clinical
examination series: Can tge clinical examination diagnose left sided heart
failure in adults?
|
||||
Increased
filling pressure
very helpful findings are radiographic redistribution and jugular venous
distension. Somewhat helpful findings are dyspnea, orthopnea, tachycardia,
decreased systolic or pulse pressure, S3, rales, and abdominojugular reflux.
Edema is helpful only when present.
Systolic
Dysfunction
very helpful findings are radiograph (cardiomegaly, redistribution), anterior
Q waves, LBBB, and abnormal apical impulse (especially if sustained).
Somewhat help ful findings are tachycardia, decreased blood pres sure or
pulse pressure, S3, rales, dyspnea, previous infarction other than anterior,
and high peak CK (post infarct). Edema and increased jugular venous pressure
are helpful if present
Diastolic
Dysfunction
very helpful finding is elevated blood pressure during the episode of
increased filling pressure. Somewhat helpful findings are obesity, lack of
tachycardia, older age, and absence of smoking or CAD. Normal radiographic
heart size is helpful if present
Approach ‘‘in patients without known systolic
dysfunction, <1 finding of increased filling pressure can exclude
diagnosis >3 findings suggests increased filling pressure. In
patients with known systolic dysfunction, absence of finding of increased
filling pressure can exclude diagnosis, >1 finding suggests
increased filling pressure. For systolic dysfunction, can exclude diagnosis
if no abnormal findings, including no sign of increased filling pressure are
present (LR 0.1). >3 findings are needed to confirm the diagnosis
(LR+ 14)’’
|
||||
Investigations
Basic
Labs CBCD, electrolytes, urea, Cr,
troponin/CK 3, BNP, D dimer, TSH, albumin.
Imaging CXR, echocardiogram (check E/A
ratio if diastolic dysfunction)
ECG
Special
Further Imaging MIBI, MUGA
Stress test to assess ischemic heart
disease
Cardiac Catherization
ABG if severe dyspnea
Diagnostic and prognostic issue
B Type natriuretic peptide
DIAGNOSIS in addition to heart
failure, BNP is also elevated with PE, pulmonary hypertension, LVH, ACS, AF,
renal failure, overload, and sepsis
|
BNP
|
Heart
Failure diagnosis
|
|
<100 pg/mL
|
Unlikely
|
|
100 to 250 pg/mL
|
Compensated LV dysfunction
|
|
250 500 pg/mL
|
HF with both diastolic and systolic
dysfunction
|
|
500 1000 pg/mL
|
Decompensate HF
|
|
>1000 pg/mL
|
High risk of substantial HF
|
Acute Management
Symptom
Control
wLMNOPw Lasix/furose mide 20 100 mg IV PRN, Morphine 2 5 mg IV PRN,
Nitroglycerin 0.4 mg SL PRN, O2, Position (upright)
Long Term Management
Diet low salt (<100 mmol/day, 1.5 2 g/day), fluid restriction (1.5 2 L/day)><100
mmol/day, 1.5 2 g/day), fluid restriction (1.5 2 L/day)
Diuretics furosemide 20 100 IV/PO daily
BID with daily adjustments (try to use smallest dose possible to allow ACE
inhibitor) + metolazone 2.5 5 mg PO 30 min before furosemide,
spironolactone 12.5 50 mg PO daily or eplerenone 25 50 mg PO daily VASODILATORS
ACE inhibitor (captopril 6.25 50 mg PO TID, enalapril 2.5 20 mg PO BID,
ramipril 2.5 10 mg PO daily, lisinopril 2.5 20 mg PO daily, perindopril 2 8 mg
PO daily). ARB (valsartan 40 160 mg PO BID, candesar tan 8 32 mg PO daily).
Hydralazine 10 mg PO QID and nitropatch 0.4 mg PO daily. b blockers (metoprolol
50 100 mg PO BID, carvedilol 3.125 25 mg PO BID, bisoprolol 2.5 10 mg PO daily)
Digitalis digoxin 0.125 0.25 mg PO daily
Treatment underlying cause CAD (CABG),
aortic stenosis (AV replacement), sleep apnea (CPAP)
Devices if ejection fraction <30 35%,
consider cardiac resynchronization therapy (CRT/biventricular pacing) + implantable
cardioerter defibrillators (ICD). Ventricular assist devices may also be
considered in selected cases of refractory HF
Treatment Issues
ACE Inhibitor hazard ratios for total
mortality 0.77 and mortality/hospitalization 0.65 for any patients with LVEF <40%.
Target dose = maximum tolerated. Contraindications include SBP <80 mmHg,
bilateral renal artery stenosis, severe renal failure, and hyperkalemia.
ARB consider substitution with ARB if
ACE inhibitor not tolerated (e.g. cough). May also be used as adjunct to ACE
inhibitor if b blocker not tolerated. Contraindications similar to ACE
inhibitor.
Hydralazin/Nitrates (VHEFT I and II, A
HeFT) less effective than ACE inhibitor. Particularly useful for pregnant
patients, African Americans, or those who developed renal insufficiency while
on ACE inhibitor, or as add on therapy
β Blockers hazard ratios for total
mortality 0.65 and mortality/hospitalization 0.64. May worsen symptoms in first
few weeks and may take up to 1 year to see full effect in LVEF. Useful for
patients with NYHA II III (and stable IV) and LVEF <40%, also NYHA I, LVEF
<40%, and post MI. Contra indications include fluid overload and severe
asthma. Start only when patient euvolaemic
Spironolactone hazard ratios for total
mortality 0.7 and mortality/ hospitalization 0.65. For patients with NYHA III
IV LVEF<35%, and on maximum treatment already. Caution in elderly and renal
failure patients as higher risk of hyperkalemia.
Digoxin hazard ratios for total mortal
ity 0.99 and mortality/hospitalization 0.92. Particularly useful for patients
with both HF and atrial fibril lation, or symptomatic HF despite maximum
treatment.
Specific Entities
Causes
of Flash Pulmonary Edema cardiac (ischemic heart disease, acute aortic
regurgitation, acute mitral regurgitation, mitral stenosis/obstruction,
arrhythmia), pulmonary (pulmonary embolism, pneumonia), renal (bilateral renal
artery stenosis), systemic (hypertension crisis, fever, sepsis, anemia, thyroid
disease)
Hypertrophic
Obstructive Cardiomyopathy (HOCM)
Pathophysiology autosomal
dominant condition with mutated cardiac sarcomere, leading to massive
ventricular hypertrophy (particularly septum). This results in left ventricular
outflow tract obstruction, mitral regurgitation, diastolic dysfunction, and
subsequently myocardial ischemia and overt heart failure. Cardiac arrhythmias
may lead to sudden death (<1%/year). Other complications include atrial fibrillation
and infective endocarditis.
Risk
Factors for Sudden Death major risk factors include history of cardiac
arrest (VF), sustained VT, unexplained syncope, non sustained VT on Holter,
abnormal BP response on exercise test, left ventri cular wall thickness >30
mm, and family history of sudden death. Minor risk factors include left ventricular
outflow obstruction (gradient >30 mmHg), microvascular obstruction,
and high risk genetic defect.
Clinical
Features
most are asymptomatic although dyspnea, chest pain, syncope, and sudden death
may develop. Family history should be obtained. Physical findings include brisk
carotid upstroke, bifid carotid pulse, double apical impulse, systolic ejection
murmur (LLSB, louder with stand ing and Valsalva) + mitral regurgitation
murmur
Diagnosis echocardiogram
(septal thickening, systolic anterior motion of mitral valve). Further workup
includes 48 h holter monitor and exercise testing annually
Treatments avoidance
(dehydration and strenuous exercise), medical (β blockers and non dihydropyridine
calcium channel blockers as first line, disopyramide as second line),
interventional/surgical (septal myomectomy, alcohol septal ablation, dual
chamber pacing), prophylaxis (implantable cardioverter defibrillator for high risk
patients to prevent sudden cardiac death, anticoagulation if atrial
fibrillation).





Comments
Post a Comment