Acute Coronary Syndrome
DIFFERENTIAL DIAGNOSIS OF CHEST
PAIN
Cardiac
Myocardial infarction, angina (atherosclerosis,
vasospasm)
Valvular aortic Stenosis
Pericardial Pericarditis
Respiratory
Parencymal pneumonia, cancer
Pleural pneumothorax, pneumomediastinum, pleural
effusion, pleuritis
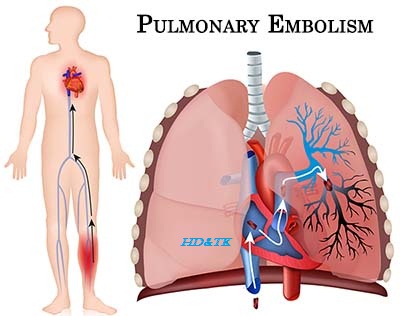
Vascular pulmonary embolism
GI esophagitis, esophageal cancer, GERD, peptic ulcer disease,
Boerhaave’s, cholecystitis, pancreatitis
Others musculoskeletal (costochondritis), shingles,
anxiety
PATHOPHYSIOLOGY
Pathologic changes
|
Clinical presentation
|
|
Pre clinical
|
Atherosclerosis
|
Asymptomatic
|
Angina
|
Luminal narrowing
|
Central chest discomfort; worsened by exertion,
emotion, and eating; relieved by rest and nitroglycerine
|
Unstable angina
|
Plaque rupture or thrombus
|
Worsening pattern or rest pain
|
NSTEMI
|
Partial occlusion
|
Non ST elevation MI
|
STEMI
|
Complete occlusion
|
ST elevation MI
|
Universal Definition of Myocardial Infarction (MI)
TYPE 1 spontaneous MI due to a primary coronary event
(atherosclerotic plaque rupture or erosion with acute thromboembolism)
TYPE 2 MI due to supply demand mismatch
TYPE 3 MI associated with sudden unexpected cardiac
death
TYPE 4 MI associated with PCI (4A) or stent thrombosis
(4B)
TYPE 5 MI associated with CABG
Risk Factors
Major diabetes, hypertension, dyslipidemia, smoking, family
history of premature CAD, advanced age, male gender
Associated obesity, metabolic syndrome, sedentary
lifestyle, high fat diet
Emerging lipoprotein abnormalities, inflammation
(increased in level CRP), chronic infections, renal failure.
Post MI Complications arrhythmia (VT/VF, bra
dycardia), sudden death, papillary muscle rupture/dysfunction, myocardial
rupture (ventricular wall, interventricular septum), ventricular aneurysm,
valvular disease (especially acute mitral regurgitation), heart failure/car
diogenic shock, pericarditis (Dressler’s syndrome)
CLINICAL FEATURES
Chest Pain Equivalents dyspnea, syncope, fatigue,
particularly in patients with diabetic neuropathy who may not experience chest
pain
New York Heart Association (NYHA) Classification
I = no symptoms with ordinary physical activity
II = mild symptoms with normal activity (walking >2
blocks or 1 flight of stairs)
III = symptoms with minimal exertion
IV = symptoms at rest
Canadian cardiovascular society (CCS) Classification
I = angina with strenuous activity
II = slight limitation, angina with meals/cold/stress
III = marked limitation, angina with walking < 1 to
2 blocks or 1 flight of stairs
IV = unstable angina
IVA= unstable angina resolves with
medical treatment
IVB = unstable angina on oral treatment,
symptoms improved but angina with minimal
provocation
IVC = unstable angina persists, not
manageable on oral treatment or hemodynamically unstable
Killip class classification
I = no evidence of heart failure
II = mild to moderate heart failure (S3, lung rales
less than half way up, or jugular venous distension)
III = overt pulmonary edema
IV = cardiogenic shock
Rational clinical examination series: Is this
patient having a myocardial infarction?
|
|
LR+
|
|
History
|
|
Radiation to right shoulder
|
2.9
|
Radiation to left arm
|
2.3
|
Radiation to both arms
|
7.1
|
Nausea or vomiting
|
1.9
|
Diaphoresis
|
2.0
|
Pleuritic chest pain
|
0.2
|
Sharp or stabbing chest pain
|
0.3
|
Positional chest pain
|
0.3
|
Chest pain reproducible by palpation
|
0.2 0.4
|
Physical
|
|
Hypotension
|
3.1
|
S3
|
3.2
|
Pulmonary crackles
|
2.1
|
ECG
|
|
New ST elevation >1 mm
|
5.7 53.9
|
New Q wave
|
5.3 24.8
|
Any ST elevation
|
11.2
|
New conduction defect
|
6.3
|
New ST depression
|
3.0 5.2
|
Any Q wave
|
3.9
|
Any ST depression
|
3.2
|
T wave peaking or inversion >1 mm
|
3.1
|
New T wave inversion
|
2.4 2.8
|
Any conduction defect
|
2.7
|
APPROACH ‘‘radiation of chest pain,
diaphoresis, hypotension, and S3 suggest acute MI. Chest pain that is
pleuritic, sharp or stabbing, positional or reproduced by palpation decreases
likelihood of acute MI. On ECG, any ST ", new Q waves, or new
conduction D make acute MI very likely. Normal ECG is very powerful to
rule out MI’’
|
|
INVESTIGATIONS
Basic
Labs CBCD, electrolytes, urea, Cr, glucose, troponin/
CK 3 q8h, AST, ALT, ALP, bilirubin, INR/PTT, Mg, Ca, PO4, albumin, lipase,
fasting lipid profile, HbA1C
Radiography
CXR, echocardiogram (first 72 h), MIBI/thallium (>5 days later)
ECG q8h 3 or with chest pain
Stress Test
ECG, echocardiogram, MIBI once stable (>48 h post MI)
Coronary Catherization
DIAGNOSTIC AND PROGNOSTIC ISSUES
Risk Stratification for stable Coronary Disease
ECG exercise test
Absolute contraindications recent
myocardial infarction (>4 days), unstable angina, severe symptomatic LV
dysfunction, life threatening arrhythmia, acute pericarditis, aortic
dissection, PE, severe symptomatic aortic Stenosis
Goal keep on treadmill until subject
reaches 85 90% of age predicted heart rate (220 age).
Ischemia Criteria >1 mm
horizontal or down sloping ST decreased level over multiple leads, or ST
increased level —> myocardial ischemia (sens 68%, spc 77%) —>
proceed to angiogram
Inclusive premature
termination due to chest pain/poor exercise tolerance —> proceed to
pharmacological stress test.
Duk Treadmill Score (exercise time in
minutes) 5x(maximum ST decreased level in mm) 4x(tread mill angina index
[0=none, 1=non limiting, 2=exercise limiting]). Low risk > 5
(4 year survival 98 99%), , moderate risk 10 to +4, high
risk < 11 (4 year survival 71 79%)
DIipyrid/Adenosive MIB dipyridamole (Per
santine) causes vasodilation. In CAD, the coronary artery is already maximally
dilated to compensate, so addition of dipyridamole will not change perfusion to
diseased vessel(s) further. This result in a relative perfusion mismatch
compared to areas with normal dilatory reaction. Contraindicated in
asthma/COPD. Antidote is aminophylline or caffeine
Dobutamine Echocardiography assesses wall motion
abnormalities. Compared to MIBI, echo cardiogram is more specific and less
sensitive. Contraindicated in severe hypertension and arrhythmias
Diagnosis of stable CAD start with history,
physical, rest ECG, and CXR. If low probability, do not investigate further. If
high probability, proceed with management. If intermediate probability —>
stress test —> cardiac CT, MIBI or stress echo —> angiography
Differential, Diagnosis of Troponin
Elevation Cardiac myocardial
infarction, myocarditis, congestive heart failure, pericarditis, vasospasm,
tachycardia with hemodynamic compromise, cocaine ingestion
Pulmonary embolism
Hepatic liver failure
Renal chronic kidney disease
Neurologic stroke, intracranial hemorrhage
Systemic sepsis, prolonged strenuous
exercise
Serum Markers
Troponin I/T rises within 4 6 h, peaks at
18 24 h, remains elevated 7 10 days (sens 40% at presentation, 40 70% after 6 9
h of symptoms)
CK/CKMB rises within 4 6 h, peaks at 18 24
h, remains elevated 3 4 days (sens 35 50% at presentation, 90% after 3 h in ER)
Myoglobin rises within 1 2 h, peaks in few
hours
TIMI Score patients with unstable
Angina/NSTEMI
Scoring (out of 7) age > 65, > 3
CAD risk factors, known CAD (stenosis > 50%), ASA use within 7 days, > 2
angina episodes within 24 h, " cardiac marker, ST deviation >0.5
mm
Risk Groups low = 0 2, intermediate = 3 4,
high = 5 7. Consider GPIIb/IIIa and early angiography with revascularization in
intermediate or high risk groups
Risk of death, MI or Revascularization in
14 days 0/1 = 5%, 2 = 8%, 3 = 13%, 4 = 20%, 5 = 26%, 6/7 = 41%
TIMI Score for patients with STEMI
Scoring (out of 14) age (3 points= > 75,
2 points=65 74), any of diabetes, hypertension, or angina (1 point), systolic
BP < 100 mmHg (3 points), HR > 100 (2 points), Killip II
IV (2 points), weight < 67 kg (1 point), anterior ST elevation or LBBB (1
point), time to reperfusion >4 h (1 point)
Risk of death in 30 dyas 0=0.8%, 1=1.6%,
2=2.2%, 3=4.4%, 4=7.3%, 5=12.4%, 6=16.1%, 7=23.4%, 8=26.8%, >8=35.9%
In Hospital Outcomes
|
||
NSTEMI
|
STEMI
|
|
Death
|
4%
|
6%
|
Reinfarction
|
0.9%
|
1.1%
|
Cardiogenic shock
|
2.8%
|
6.4%
|
Stroke
|
0.7%
|
0.8%
|
Major bleeding
|
10%
|
12%
|
ACUTE
MANAGEMENT
ABC O2 to keep sat >95%, IVs,
inotropes, consider balloon pump if hemodynamic instability
Pain Control nitroglycerin
(nitro drip 25 mg in 250 mL D5W, start at 5 mg/min IV, then increased by 5 by 5
10 mg/ min every 3 5 min to 20 mg/min, then increased by 10 mg/ min every 3 5
min up to 200 mg/min, or until relief of pain, stop titration if SBP is <
100 mmHg. Nitro patch 0.4 mg/h daily. Nitro spray 0.4 mg SL q5min x3. Beware if
suspect right ventricular infarction or if patients on sildenafil). Morphine 2
4 mg IV every 5 15 min PRN.
Clot Control
Antiplatelet ASA 162 325 mg PO chew x 1
dose, then 75 162 mg PO daily (for medically treated unstable angina/NSTEMI),
or 162 325 mg PO daily (post PCI minimum x 1 month for bare metal stent, x 3
months for sirolimus eluting stent, or x 6 months for paclitaxeleluting stent),
then 75 162 mg PO daily indefinitely. If NSTEMI or STEMI, clopidogrel 300 600
mg x1 dose then 75 mg PO daily. Combination ASA plus clopidogrel for minimum of
1 month (ideally 1 year) post PCI with bare metal stent, or minimum 12 months
(possibly indefinitely) for drug eluting stents. If post PCI, pain unresponsive
to nitroglycerin or intermediate/high risk NSTEMI, consider GPIIb/IIIa
inhibitor (tirofiban 0.4 mg/kg/min 30 min IV, then continue 0.1 mg/kg/min
x 18 24 h after angioplasty/atherectomy. Eptifibatide 180 mg/kg IV bolus, then
2 mg/kg/min x 72 96 h)
Anticoagulation options include LMWH
(enoxaparin 30 mg IV bolus, then 1 mg/kg SC BID for STEMI [no IV bolus for
NSTEMI caution if renal failure or age > 5) or unfractionated heparin
(unfractionated heparin 70 U/kg [up to 4000U] IV bolus, then 18 U/kg/hr [up to
1000U/h] and adjust to 1.5 2.5 x normal PTT for 72 h). Factor Xa inhibitors
(Fondaparinux 2.5 mg SC daily until discharge or 8 days, caution if renal
failure). Direct thrombin inhibitors (Bivalirudin 0.1 mg/kg IV bolus then 0.25
mg/kg/hr initially, followed by second 0.5 mg/kg bolus before PCI and 1.75 mg/
kg/hr during PCI, then continue infusion for up to 4 h post PCI, if needed)
Rate Control IV metoprolol is mostly
contra indicated. Start with metoprolol 25 mg PO BID and titrate slowly.
Alternatively, atenolol 25 mg PO daily and titrate to 100 mg PO daily. The goal
heart rate is 50 55 with normal activity. If b blocker contraindicated,
consider non dihydropyridine calcium channel blockers diltiazem 30 120 mg PO
QID or verapamil 80 120 mg PO TID (contraindicated if LV dysfunction)
Lipid Control simvastatin 40 mg PO daily
or atorvastatin 80 mg PO daily
Blood Pressure Support for patients with
cardiogenic shock, consider IV fluids, inotropes (dobutamine/dopamine), balloon
pump, and early revascularization
Cautions in treatment of acute myocardial
infarction avoid
negative inotropic agents such as b blockers and non dihydropyridine calcium
channel blockers if clinical heart failure. Avoid administration of
nitroglycerin, morphine, and diuretics to patients with right ventricular
infarction as these medications can cause venodilation and decrease preload,
leading to hypotension.
LONG TERM MANAGEMENT OF CORONARY ARTERY DISEASE
Antianginal nitroglycerin (nitro patch
0.4 0.8 mg/h daily; nitro spray 0.4 mg SL q5min 3; isosorbide mononitrate 30 mg PO daily, maximum 240 mg), b
blocker (metoprolol 25 100 mg PO BID, atenolol 50 100 mg PO daily, bisoprolol 5
10 mg PO daily), calcium channel blocker (amlodipine 5 10 mg PO daily)
ACE Inhibitor ramipril 2.5 10 mg PO daily
Ant platelet ECASA 81 mg PO daily and/or
clo pidogrel 75 mg PO daily
Anticoagulation controversial especially
in combination with ASA and/or clopidogrel. May be considered for patients post
STEMI or NSTEMI with one of the following criteria: (1) atrial fibrillation,
(2) left ventricular thrombus, (3) significant left ventricu lar dysfunction
with extensive regional wall motion abnormalities. Start warfarin 5 mg daily
within 72 hours and continue heparin/LMWH until INR is between 2 and 3 (unless
planning angioplasty)
Risk
Reduction
ASA/ACE Inhibitor
Blood Pressure Control
Cholesterol Control
Diabetic Control
Exercise (30 min of moderate intensity
exercise 3 4x /week)
Fat Redyction
Get going to quit smoking!
TREATMENT ISSUES
Right Ventricular Infarction evidence of
inferior MI should automatically trigger one to check right sided leads (V4R)
to assess for the possibility of RV infarction, which occurs in about 50% of
patients with inferior MI.
Posterior Infarction ST depression in V1
V2 in a regular ECG should automatically trigger one to request for posterior
(V7 V9) leads to check for posterior MI. Posterior infarct may be associated
with inferior infarcts (90%) and lateral infarcts (10%) as the PDA may be
supplied by the right or left circum flex coronary artery
Post
MI Risk Stratification
Extent of Infarct/Residual Function
assessment is based on clinical factors (raised HR, decreased BP, Killip class,
diabetes, renal failure, raised WBC), ECG, biomarkers (CK, troponin), imaging
(echocardiogram, MIBI), and angiography. Early measurement of LV function,
although of prognostic importance, is misleading as myocardium function may
improve in first 2 weeks. Medical management
Extent of Myocardium at risk assessment
is based on exercise stress test, stress echocardiogram, stress sestamibi
(ischemic tissue), thallium scan (viable tissue), PET scan, angiography. Angioplasty
or CABG should be considered.
Risk of Arrhythmia high risk of VF/VT
within the first 48 h, therefore monitor with telemetry. If it occurs after 48
h, consider antiarrhythmics and early ICD
Balloon Pump a long balloon in the
descending aorta that deflates during systole and inflates during diastole to
augment coronary perfusion and cardiac output as well as decrease after load.
Indicated if cardiogenic shock with hemodynamic instability. May be used in
conjunction with inotropes. Contra indicated in aortic regurgitation, AAA,
aortic dissection, uncontrolled sepsis bleeding disorder, and severe PVD
Fibrinolytics
use (TPA, SK, RPA, TNK)
Indications > 30 min of chest
pain, patient presents within 12 h (ideal door to needle time < 30 min), ECG
criteria (>1 mm ST " in > 2 contiguous leads, or new LBBB
with suggestive history, age < 75)
Absolute Contraindications any
intracranial hemorrhage, ischemic stroke within 3 months, cerebral vascular
malformation or brain tumor, closed head or facial trauma within 3 months,
suspected aortic dissection, bleeding diathesis, or active bleeding
Relative Contraindications severe
hypertension (>180/110 mmHg, may be an absolute contraindication for patients
at low risk), ischemic stroke > 3 months, other intracranial diseases not
already specified above, dementia, internal bleeding within 2 4 weeks, active
peptic ulcer, major surgery within 3 weeks, non compressible vascular
punctures, cur rent warfarin therapy, pregnancy, traumatic CPR > 10 min,
prior exposure to streptokinase or anistreplase (if planning to use these
fibrinolytics)
Risk of Bleeding average risk of severe
bleed is 1.8%. Increased risk with women, BP > 165/ 95 mmHg, age > 65,
weight < 70 kg [<154lbs], and electrolysis with TPA (+0.5% absolute
risk/factor)
Persistent ST Elevation look for
resolution of symptoms and ST elevation to decrease by >50% within 90 min of
fibrinolytic therapy. Persistent ST elevation may suggest failed fibrinolytic
therapy, and require urgent rescue catheterization. Other causes of ST elevation
include pericarditis, ventricular aneurysm, hyperkalemia, LBBB, and early
repolarization abnormality.
Percutaneous
Coronary Intervention (PCI, PTCA)
Indication for acute STEMI patient
presents within 12 h of chest pain (ideal time from initial medical contact to
treatment or ‘‘door to balloon time ’ < 90 min), ECG criteria (>1 mm ST
increased in > 2 contiguous leads, new or presumed new left bundle
branch block), or in patients in cardiogenic shock within 18 h of infarct
Indications for Chronic Stable CAD
single/ double vessel disease refractory to medical therapy.
Adverse events access site (bleeding,
hematomas, arteriovenous fistulae, pseudoaneurysms), contrast nephropathy,
arrhythmia (VT, VF), stroke, dissection, myocardial infarction.
Bare metal Stents vs. Drug-Eluting
Stents in stent restenosis is due to fibrosis of coronary vasculature and
usually happens 3 months post procedure. Drug eluting stents (sirolimus or
pacli taxel) are designed to inhibit cell proliferation and decrease the risk
of in stent restenosis. There has been some controversy regarding higher
observed mortality rate in patients with drug eluting stents. The most recent
outcomes research analysis suggests that drug eluting stents are associated
with decreased rate of repeat revascularization (19% vs. 23%, HR 0.82) at 2
years and no significant difference in mortal ity (8.4% vs. 8.4%)
Benefits primary PCI is generally
preferred given the superior outcomes compared to fibrinolysis, particularly if
(1) fibrinolysis contraindicated, (2) previous history of CABG, or (3) cardiogenic
shock. However, patients who were able to seek medical attention within 1 h of
chest pain onset, allergic to contrast dye, or do not have access to PCI in a
timely fashion should consider fibrinolytics
Coronary
Artery Bypass Graft Surgery
Coronary Anatomy
Right Coronary Anatomy (RCA) gives rise
to right marginal (RMA), right posterior descending (RPDA), and right
posterolateral branches (RPL 1, 2, 3)
Left Main (LM) gives rise to left
anterior descending (LAD) ͢ ! diagonal
(D1, 2 3) and septals; ramus intermediate (Ram Int); and left circum flex (LCX)
͢ obtuse marginal (OM 1, 2, 3)
Dominant Artery defined as the artery
that sup plies PDA and at least one posterolateral (PL) artery
Indications CABG provides mortality benefit for specific
subgroups, including patients with
1) left main disease >50% occlusion,
2) 2 vessel disease with significant
involvement of proximal left anterior descending, and
3) diffuse triple vessel disease. Diabetic
patients and those with reduced left ventricular function derive more benefit
from bypass surgery
Morbidity
Benefit 95% have improvement of symptoms
immediately after surgery, 75% symptom free at 5 years. Recurrent disease more
common in vein grafts than artery grafts
Grafts
saphenous
veins from calf or thigh (SVG), internal mammary arteries (LIMA/RIMA), radial
arteries (RA), and gastroepiploic artery from sto mach (GA). A total of 90% of
arterial graft and 50% of vein graft remain patent by 10 years
Complications
Cardiac MI 2 4%, arrhythmia (AF 40%,
sustained VT/VF 2 3%), AV block requiring pacemaker 0.8 4%,
pericarditis/tamponade, aortic dissection
Neurological stroke, postoperative
delirium, cognitive impairment, depression, phrenic nerve damage, intercostal
nerve damage
Others renal failure, bleeding,
infection, pleural effusions
Medications hold clopidogrel 5 7 days
prior to CABG. Continue ASA before and after surgery.





Comments
Post a Comment